CONTRAINDICATIONS
- Patients unable to tolerate vascular occlusion procedures.
- Vascular anatomy precluding correct catheter placement. - Feeding arteries too small to accept the selected microspheres.
- Presence or suspicion of vasospasm.
- Presence of distal arteries directly supplying cranial nerves.
- Presence of patent extra-to-intracranial anastomoses.
- High-flow arteriovenous shunts or with a diameter greater than the selected microspheres. - Use in the pulmonary vasculature. - Severe atherosclerosis.
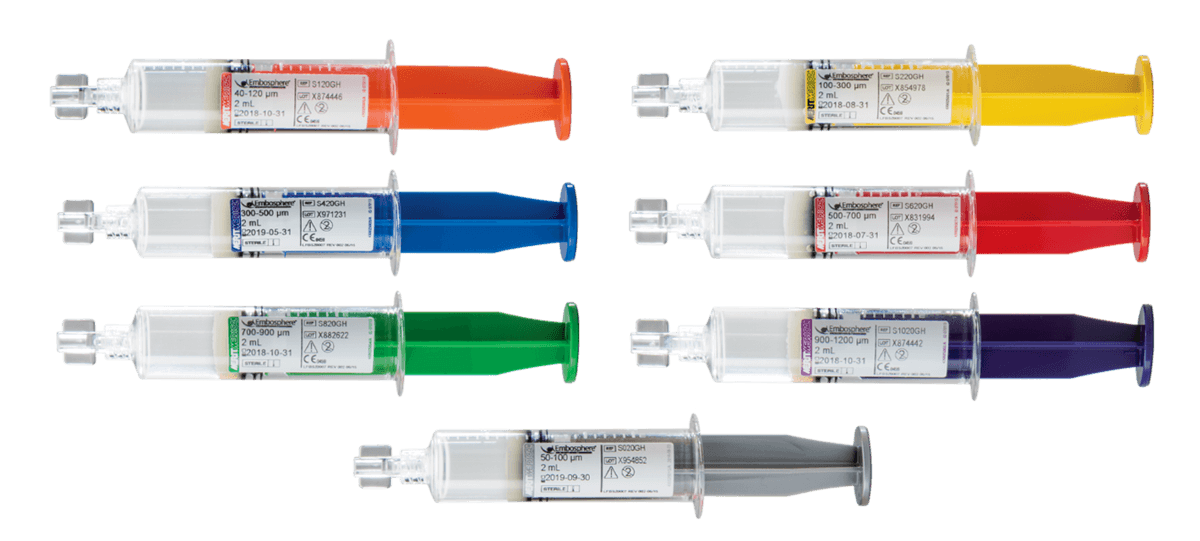
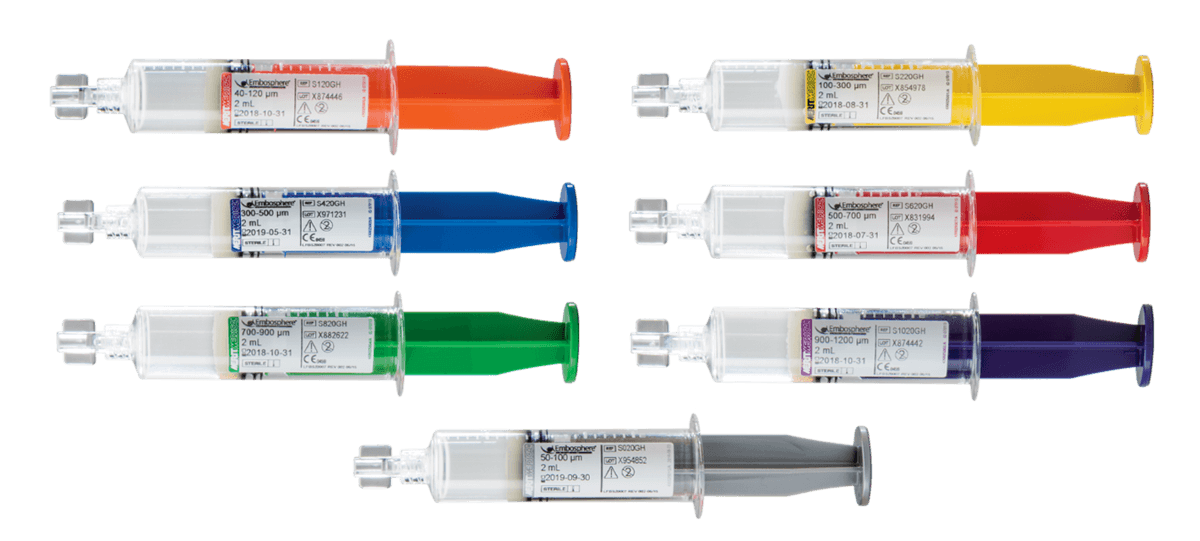
- Patients with known allergy to gelatin. 50-100 µm, 40-120 μm and 100-300 μm microspheres are not recommended for use in the bronchial circulation.
CAUTION
DO NOT USE THIS PREFILLED SYRINGE TO DIRECTLY INJECT EMBOSPHERE MICROSPHERES. THIS IS A “RESERVOIR” SYRINGE. PLEASE REFER TO INSTRUCTIONS PARAGRAPH.
Embosphere Microspheres must only be used by specialist physicians trained in vascular embolisation procedures. The size and quantity of microspheres must be carefully selected according to the lesion to be treated, entirely under the physician’s responsibility. Only the physician can decide the most appropriate time to stop the injection of microspheres.
Do not use if blister tray, peel-away film, screw cap or syringe are damaged. This is a disposable product. Discard opened syringes after use. All procedures must be performed according to an aseptic technique.
For single patient use only - Contents supplied sterile Do not reuse, reprocess, or resterilise. Reusing, reprocessing or resterilising may compromise the structural integrity of the device and or lead to device failure, which in turn may result in patient injury, illness or death. Reusing, reprocessing or resterilising may also create a risk of contamination of the device and or cause patient infection or cross infection including, but not limited to, the transmission of infectious disease(s) from one patient to another. Contamination of the device may lead to injury, illness or death of the patient.
WARNINGS
• Embosphere Microspheres contain gelatin of porcine origin, and therefore, could cause an immune reaction in patients who are hypersensitive to collagen or gelatin. Careful consideration should be given prior to using this product in patients who are suspected to be allergic to injections containing gelatin stabilizers.
• Studies have shown that Embosphere Microspheres do not form aggregates, and, as a result, penetrate deeper into the vasculature as compared to similarly sized PVA particles. Care must be taken to choose larger sized Embosphere Microspheres when embolising arteriovenous malformations with large shunts to avoid passage of the spheres into the pulmonary or coronary circulation.
• Some of the Embosphere Microspheres may be slightly outside of the range, so the physician should be sure to carefully select the size of Embosphere Microspheres according to the size of the target vessels at the desired level of occlusion in the vasculature and after consideration of the arteriovenous angiographic appearance. Embosphere Microspheres size should be selected to prevent passage from artery to vein.
• Because of the significant complications of misembolisation, extreme caution should be used for any procedures involving the extracranial circulation encompassing the head and neck, and the physician should carefully weigh the potential benefits of using embolisation against the risks and potential complications of the procedure. These complications can include blindness, hearing loss, loss of smell, paralysis and death. • Because of the tortuous vessels and duplicative feeding arteries in the pelvic area, extreme caution should be used when performing embolisation for the treatment of symptomatic Benign Prostatic Hyperplasia. Complications of misembolisation may include ischaemia of the rectum, bladder, scrotum penis or other areas.
• Serious radiation induced skin injury may occur to the patient due to long periods of fluoroscopic exposure, large patient diameter, angled x-ray projections, and multiple image recording runs or radiographs. Refer to your facility’s clinical protocol to ensure the proper radiation dose is applied for each specific type of procedure performed. Physicians should monitor patients that may be at risk.
• Onset of radiation-induced injury to the patient may be delayed. Patients should be counseled on potential radiation side effects and whom they should contact if they show symptoms.
• Pay careful attention for signs of mistargeted embolisation. During injection carefully monitor patient vital signs to include SaO2 (e.g. hypoxia, CNS changes). Consider terminating the procedure, investigating for possible shunting, or increasing microsphere size if any signs of mistargeting occur or patient symptoms develop.
• Consider upsizing the microspheres if angiographic evidence of embolisation does not quickly appear evident during injection of the microspheres.