Manufacturer > BD > Devices > Lutonix™ 035 DCB – Dysfunctional AV Fistula Indication
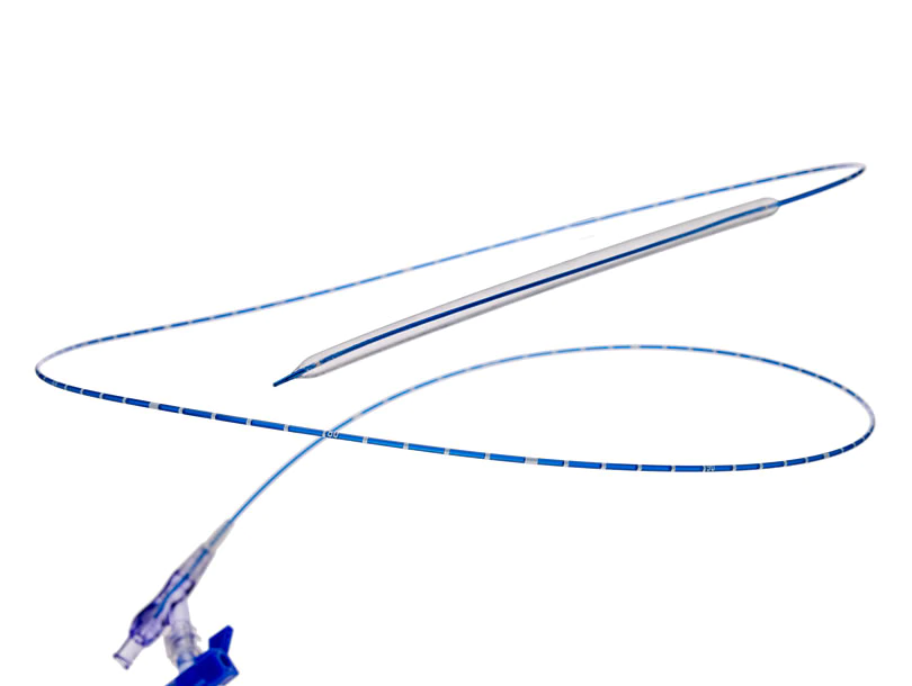
Lutonix™ 035 DCB – Dysfunctional AV Fistula Indication
1 Lutonix™ AV Clinical Trial data on file. N=285. At 6 months, treatment with Lutonix™ 035 DCB resulted in a primary patency rate of 71.4% versus 63.0% with PTA alone. Primary patency defined as ending with a clinically driven re-intervention of the target lesion or access thrombosis. The primary effectiveness analysis for superiority of DCB vs. PTA was not met with a one sided p-value of p = 0.0562. Number of interventions required to maintain TLP at 6 months were 44 in DCB arm versus 64 in the PTA arm. At 30 days, treatment with Lutonix™ 035 resulted in a freedom from primary safety event rate of 95.0% versus 95.8% with PTA alone. Primary safety defined as freedom from localized or systemic serious adverse events through 30 days that reasonably suggests the involvement of the AV access circuit. The primary safety endpoint for noninferiority for DCB vs. PTA was met with one-sided p-value of p = 0.0019. Percentages reported are derived from Kaplan-Meier analyses. Mean time to TLPP event for subjects with an event was longer for DCBs (321.8 vs. 207.4 d; p<.0001)
2 Warnings: A signal for increased risk of late mortality has been identified following the use of paclitaxel-coated balloons and paclitaxel-eluting stents for femoropopliteal arterial disease beginning approximately 2-3 years post-treatment compared with the use of non-drug coated devices. There is uncertainty regarding the magnitude and mechanism for the increased late mortality risk, including the impact of repeat paclitaxel device exposure. Inadequate information is available to evaluate the potential mortality risk associated with the use of paclitaxel-coated devices for the treatment of other diseases/conditions, including this device indicated for use in arteriovenous dialysis fistulae. Physicians should discuss this late mortality signal and the benefits and risks of available treatment options with their patients.
Lutonix™ 035 Drug Coated Balloon PTA Catheter Indications for Use: The Lutonix™ Catheter is indicated for percutaneous transluminal angioplasty (PTA), after pre-dilatation, for treatment of stenotic lesions of dysfunctional native arteriovenous dialysis fistulae that are 4 mm to 12 mm in diameter and up to 80 mm in length.
Please consult Instructions for Use for product indications for use, contraindications, warnings, precautions, complications, adverse events and detailed safety information. ℞ only
Features and Benefits
Device Documents
Questions & Answers